Reflections from the 4th International Research Seminar: EAPC Reference Group on Public Health and Palliative Care, University of Victoria June 17-19 2025
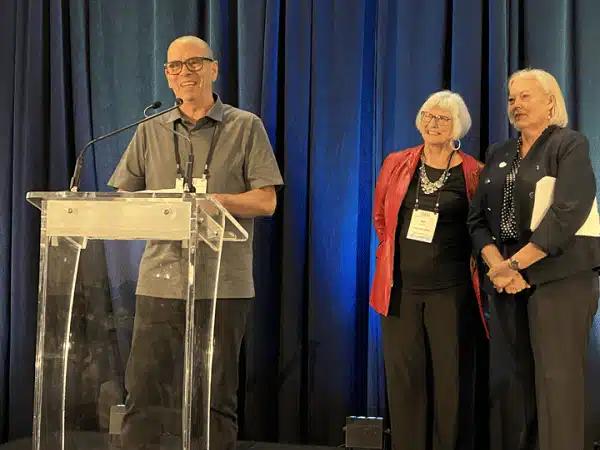
By: Dawn Elston – Life and Death MattersFeatured Photo: Drs Leah Norgrove, Ambrose Marsh, Fraser Black, and Kath Murray and Coby Tschanz This year’s European